Healthcare Payers (P1) Focused Enterprise Software Products & Platforms
Healthcare Payers (P1) Focused Enterprise Software Products & Platforms
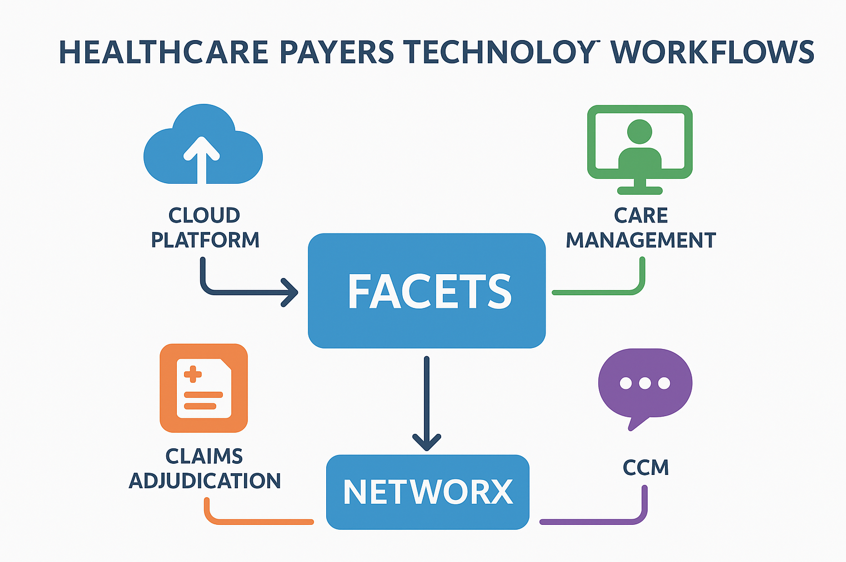
The U.S. healthcare payer ecosystem is one of the most complex in the world, with health plans managing claims, enrollment, billing, compliance, provider networks, and member engagement across millions of lives. Enterprise software products and platforms play a pivotal role in ensuring payers can deliver efficient, compliant, and member-centric services. Cognizant’s TriZetto suite of products—including Facets, QNXT, CCA, TCS, and NetworX Pricer—are widely adopted across payer organizations to power critical workflows.
-
1. The U.S. Payer World
Healthcare payers (P1) include commercial insurers, Blue Cross Blue Shield plans, Medicaid MCOs, and Medicare Advantage plans. Their core operations include:
- - Enrollment & Eligibility
- - Premium Billing
- - Claims Adjudication & Payment
- - Provider Network & Pricing
- - Care Management (UM/CM/DM)
- - Appeals & Grievances
- - Compliance & Regulatory Reporting
Given the scale and complexity of payer operations, enterprise-grade platforms are necessary to support integration, automation, and digital transformation.
-
2. TriZetto Products and Platforms
- - Facets: Enterprise core administration platform for claims, enrollment, billing, and benefits configuration.
- - QNXT: Rules-driven payer platform with scalability for mid-large payers.
- - CareAdvance (CCA): Care management solution enabling utilization, case, and disease management workflows.
- - TCS (TriZetto Communication Services): Manages multi-channel communications to providers and members, ensuring compliance and CCM support.
- - NetworX Pricer: Pricing engine for provider contracts, Medicare/Medicaid reimbursement, and value-based models.
-
3. Role of TriZetto in Payer Workflows
- - Facets: Enables automated claims adjudication, reducing manual intervention and increasing first-pass resolution rates.
- - CCA: Supports integrated UM/CM/DM workflows, ensuring compliance with NCQA/URAC standards.
- - TCS: Delivers compliant, automated communications (letters, emails, SMS) for claims, appeals, and authorizations.
- - NetworX: Provides flexible contract configuration, pricing accuracy, and cost savings for payers.
- - QNXT: Often used by Medicaid and Medicare plans requiring rules-based configurations.
-
4. Digital Transformation & Alignment
Modern payers are embracing digital transformation to reduce administrative costs, meet CMS regulations, and improve member experience. Platforms like TriZetto enable API-driven integration, advanced analytics, and cloud hosting. By aligning business strategy (cost containment, regulatory compliance, and member engagement) with technology investments, payers can achieve significant operational efficiency.
Hashtags
#HealthcarePayers #TriZetto #Facets #QNXT #CCA #TCS #NetworX #ClaimsProcessing #DigitalTransformation #HealthcareIT #PayerIntegration #CareManagement #CCM #CMSCompliance #DataMigration