AI, GenAI, Agent AI, and Agentic AI in the Healthcare Payer World
AI, GenAI, Agent AI, and Agentic AI in the Healthcare Payer World
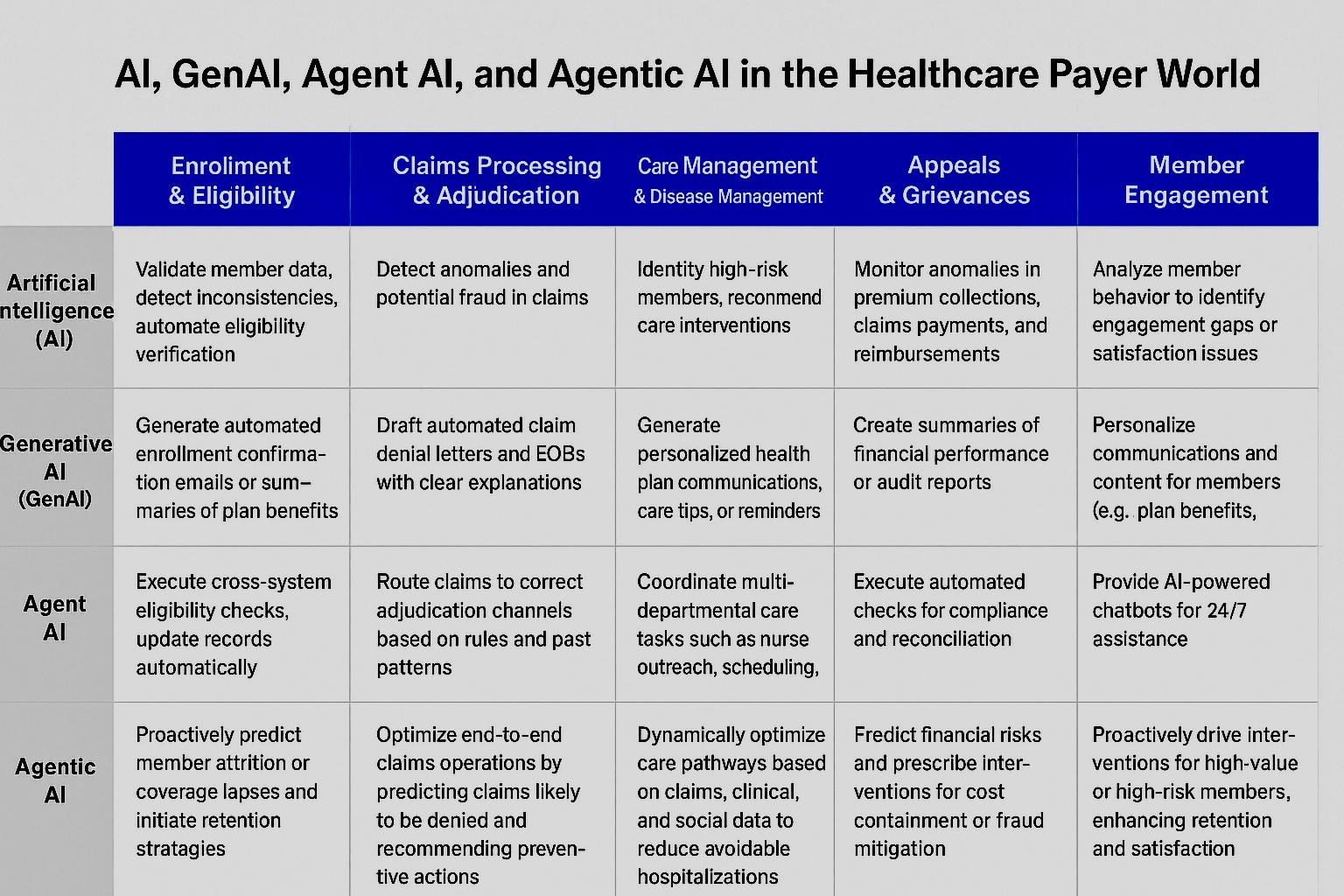
The healthcare payer ecosystem in the United States is complex, encompassing insurance enrollment, eligibility verification, claims processing, care management, financial integrity, regulatory compliance, and member engagement. The growing adoption of AI-driven technologies is reshaping how payers operate, optimize workflows, and enhance member outcomes. From traditional AI to agentic AI, these technologies are increasingly embedded in every aspect of payer operations.

-
1. Understanding the AI Spectrum in Healthcare Payers
-
1.1 Artificial Intelligence (AI)
AI refers to systems that analyze structured and unstructured data to deliver actionable insights, automate tasks, and support decision-making. In payer workflows, AI can detect anomalies in claims, predict membership churn, and identify care gaps.
Example Use Cases:
- - Claims adjudication using predictive models for fraud detection.
- - Risk scoring for members with chronic conditions.
- - Automating repetitive tasks in premium billing and reporting.

-
1.2 Generative AI (GenAI)
GenAI creates new content from existing data, including text, summaries, or predictive models. Within payers, GenAI can assist in generating member communications, summarizing complex case data, and supporting compliance documentation.
Example Use Cases:
- - Auto-generation of explanation of benefits (EOBs) with personalized summaries.
- - Creating educational content for members with chronic conditions.
- - Drafting regulatory reports or letters for enrollment, appeals, and grievances.
-
1.3 Agent AI
Agent AI is focused on autonomous agents capable of executing tasks with minimal human supervision. For healthcare payers, this means automating end-to-end operational workflows across systems.
Example Use Cases:
- - Automated verification of eligibility by querying multiple sources.
- - Intelligent claim routing and adjudication.
- - Virtual assistants for member inquiries or provider support.
-
1.4 Agentic AI
Agentic AI extends Agent AI with higher-order decision-making, planning, and adaptive learning. It can proactively identify opportunities, optimize interventions, and drive enterprise-wide decisions in real time.
Example Use Cases:
- - Predicting claim denials and proactively suggesting corrections before submission.
- - Optimizing provider networks and care management strategies using predictive modeling.
- - Real-time intervention for high-risk members by integrating claims, clinical, and social determinants data.
-
2. AI Applications Across Healthcare Payer Workflows
Healthcare payers operate through multiple interconnected workflows. Here’s a detailed mapping of AI, GenAI, and Agentic AI applications to each workflow:
-
2.1 Enrollment & Eligibility
- - AI: Validate member data, detect inconsistencies, and automate eligibility verification.
- - GenAI: Generate automated enrollment confirmation emails or summaries of plan benefits.
- - Agent AI: Execute cross-system eligibility checks, update records automatically.
- - Agentic AI: Proactively predict member attrition or coverage lapses and initiate retention strategies.
- 2.2 Claims Processing & Adjudication
- - AI: Detect anomalies and potential fraud in claims using predictive models.
- - GenAI: Draft automated claim denial letters and EOBs with clear explanations.
- - Agent AI: Route claims to correct adjudication channels based on rules and past patterns.
- - Agentic AI: Optimize end-to-end claims operations by predicting claims likely to be denied and recommending preventive actions.
-
2.3 Care Management & Disease Management
- - AI: Identify high-risk members and recommend care interventions.
- - GenAI: Generate personalized health plan communications, care tips, or reminders.
- - Agent AI: Coordinate multi-departmental care tasks such as nurse outreach, scheduling, and follow-ups.
- - Agentic AI: Dynamically optimize care pathways based on claims, clinical, and social data to reduce avoidable hospitalizations.
-
2.4 Financial Integrity & Risk Management
- - AI: Monitor anomalies in premium collections, claims payments, and reimbursements.
- - GenAI: Create summaries of financial performance or audit reports.
- - Agent AI: Execute automated checks for compliance and reconciliation.
- - Agentic AI: Predict financial risks and prescribe interventions for cost containment or fraud mitigation.
-
2.5 Appeals & Grievances
- - AI: Categorize cases and predict likelihood of approval or escalation.
- - GenAI: Generate draft responses or summary reports for regulatory submissions.
- - Agent AI: Route appeals automatically to the appropriate reviewer or department.
- - Agentic AI: Recommend strategy for high-volume or high-risk appeals, optimizing outcomes and compliance.
-
2.6 Member Engagement & Experience
- - AI: Analyze member behavior to identify engagement gaps or satisfaction issues.
- - GenAI: Personalize communications and content for members (e.g., plan benefits, health tips).
- - Agent AI: Provide AI-powered chatbots for 24/7 assistance.
- - Agentic AI: Proactively drive interventions for high-value or high-risk members, enhancing retention and satisfaction.

-
3. Benefits of Integrating AI Across Payer Workflows
- - Operational Efficiency: Automates repetitive tasks, reduces processing times, and minimizes errors.
- - Enhanced Member Experience: Personalized communication and proactive interventions increase member satisfaction.
- - Regulatory Compliance: AI supports adherence to CMS, HIPAA, and other regulations by automating reporting and monitoring.
- - Cost Optimization: Identifies fraud, predicts claim denials, and optimizes care management programs to reduce unnecessary expenditures.
- - Data-Driven Decision Making: Agentic AI enables real-time decision-making and strategic interventions across the enterprise.

-
4. Concluding Perspective
The integration of AI, GenAI, Agent AI, and Agentic AI represents a transformative opportunity for healthcare payers. From automating claims to proactively managing member health, these technologies are creating a more agile, intelligent, and patient-centric payer ecosystem. Leaders in the payer space are increasingly leveraging AI-driven insights to optimize costs, enhance member experience, and ensure compliance, ultimately redefining how healthcare plans deliver value.
We should connect. We could talk about market trends and explore business synergies, if any.
Monika Vashishtha, MBA, ITIL, PMP
President & COO
https://ghit.digital I +1 201.792.8924