Healthcare payers face increasing challenges today, from higher claims volumes to stricter regulations and growing member expectations for quick, transparent service. Legacy systems, while robust, often lack the flexibility and speed to adapt to these pressures.
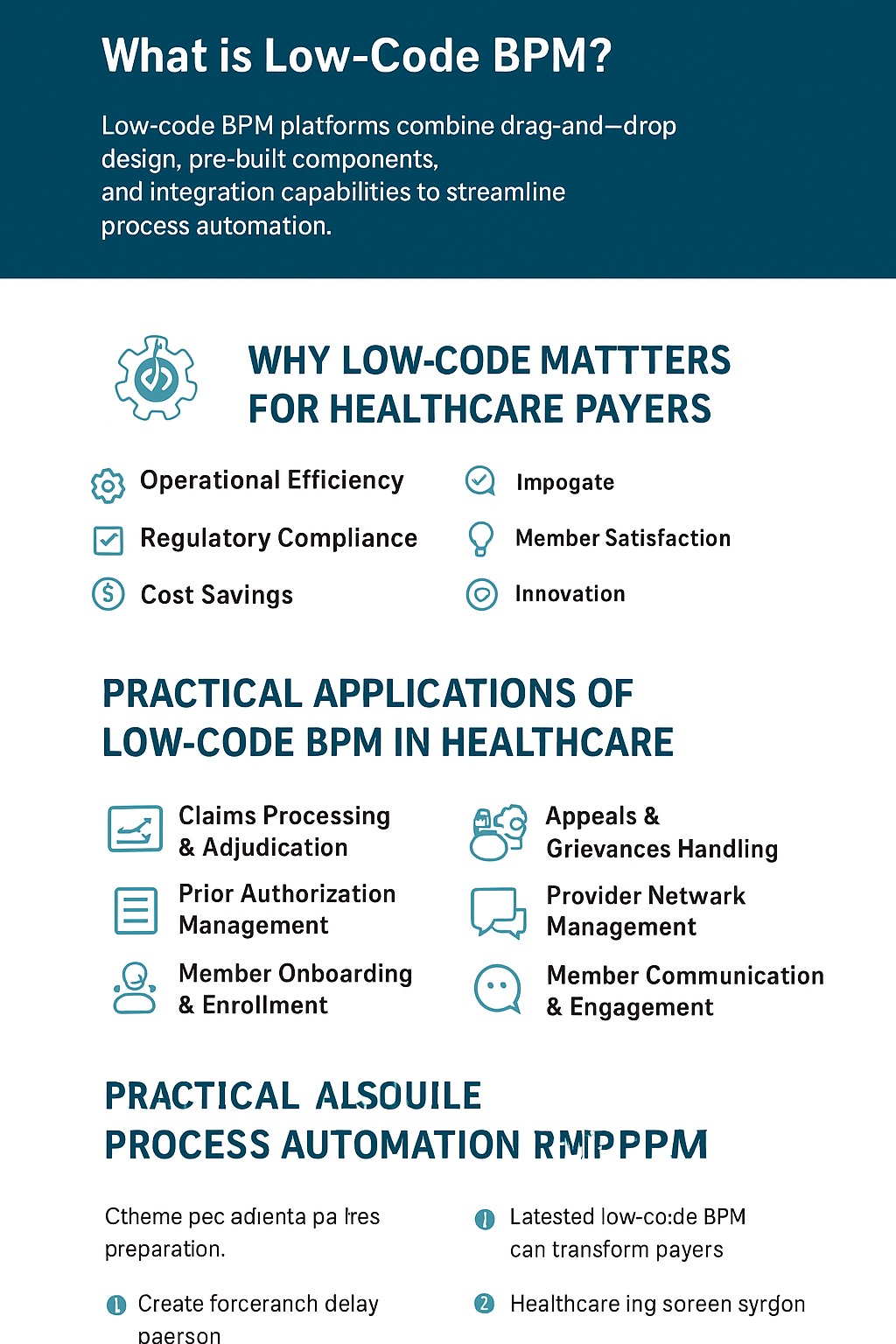
This is where low-code Business Process Management (BPM) platforms provide a modern solution. By allowing organizations to build and automate workflows with minimal coding, low-code BPM helps payers accelerate digital transformation, reduce costs, and improve the overall member experience.
In this article, we’ll take a deep dive into low-code process automation and explore practical use cases where healthcare payers are already seeing measurable impact.
Low-code BPM platforms combine drag-and-drop design, pre-built components, and integration capabilities to streamline process automation. Unlike traditional development, low-code enables:
- Faster deployment of new workflows and applications.
- Agility to adapt quickly to regulatory or market changes.
- Reduced dependency on large IT teams.
- Scalable automation that spans claims, compliance, member services, and more.
For payers, this means less time spent wrestling with legacy systems and more time focusing on strategic initiatives.
Low-code BPM addresses several critical pain points for healthcare payers:
- Operational Efficiency: Automating manual processes reduces errors and turnaround times.
- Regulatory Compliance: Built-in checks and audit trails simplify adherence to CMS, HIPAA, and other standards.
- Cost Savings: Lower reliance on custom development and faster time-to-market reduce IT spending.
- Member Satisfaction: Faster claims processing and personalized communication improve engagement and trust.
- Innovation: Payers can pilot and scale new offerings without years of system overhauls.
Low-code platforms can automate the entire claims lifecycle, from intake and validation to adjudication. This automation flags exceptions for human review while accelerating routine approvals, which helps reduce manual errors and speeds up payment cycles.
Workflows can streamline prior authorization requests by integrating provider submissions, clinical guidelines, and approval routing. This reduces delays in patient care and eases the administrative burden on providers.
Automated onboarding ensures new members are seamlessly guided through benefits selection, documentation, and coverage activation, creating a positive first impression and improving engagement.
With evolving mandates like CMS interoperability and HIPAA updates, low-code BPM can embed compliance checks directly into workflows, generate automated reports, and maintain complete audit trails for readiness.
Automated case routing, communication templates, and SLA tracking ensure appeals and grievances are resolved fairly, transparently, and on time, which improves trust and minimizes compliance risks.
Low-code automation simplifies credentialing, contract management, and ongoing monitoring, helping payers maintain accurate provider directories and meet compliance requirements with less effort.
Through integration with Customer Communication Management (CCM) systems, payers can deliver timely, personalized updates via email, SMS, or secure portals. This improves transparency and overall member satisfaction.
As payers adopt value-based care models and expand digital health ecosystems, low-code BPM will continue to evolve as a key enabler. Its ability to quickly design, test, and scale solutions means payers can stay ahead of market changes while keeping operational costs in check.
In the long run, low-code platforms won't just automate existing workflows—they'll also drive data-driven decision-making, predictive analytics, and member-centric innovations across the payer landscape.
Healthcare payers can no longer rely on outdated, manual processes. Low-code BPM offers a powerful, flexible, and cost-effective way to modernize operations, meet compliance requirements, and deliver the seamless experiences members now expect.
By embracing low-code automation today, payers can unlock new levels of efficiency, agility, and competitiveness in a rapidly evolving healthcare ecosystem.
Looking to explore how low-code BPM can transform your healthcare payer organization?
GHIT Digital, a trusted NewgenOne partner, helps payers streamline claims, compliance, and member engagement using modern automation platforms.
Contact us today for a discovery conversation or personalized demo:
- Website: GHIT.digital
- Email: Monika@GHIT.digital
Phone: 201.792.8924 | 646.734.6482