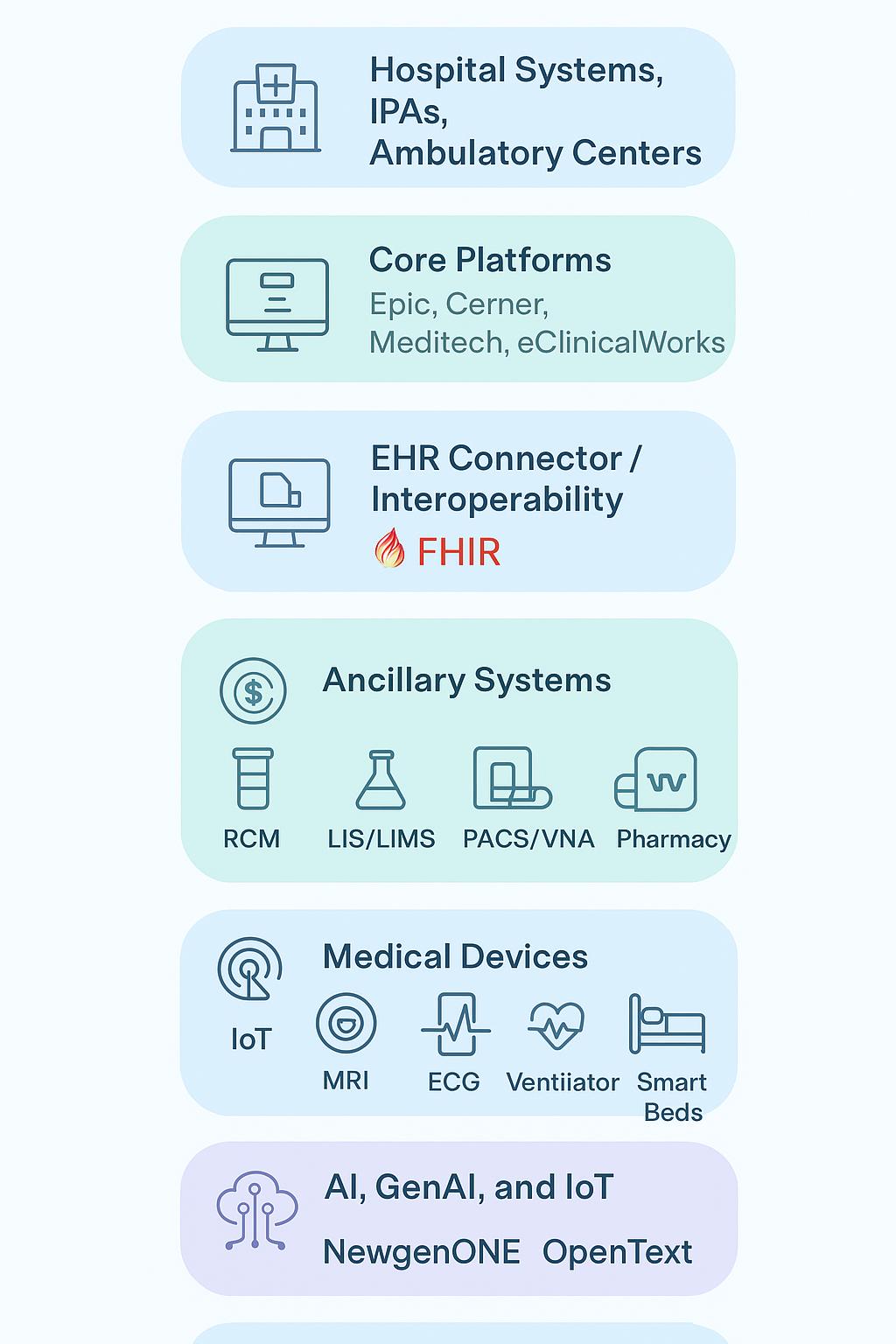
Hospitals, health systems, and Independent Practice Associations (IPAs) operate interconnected clinical, administrative, and operational workflows. While EHR/EMR platforms such as Epic, Oracle Cerner, Meditech, and eClinicalWorks form the clinical backbone, modern provider IT demands focus in three critical areas:
- EHR connector strategies to unify multi-vendor environments during acquisitions, mergers, or federated operations.
- EHR archival management to store, search, and govern legacy clinical data efficiently.
- Full medical device and IoT integration — from MRI/CT scanners to infusion pumps and RTLS assets — enabling both real-time care delivery and analytical insights.
GHIT Digital’s Point of View: Adopt a data-first integration fabric (FHIR façade with a canonical data lake), enable low-code orchestration for cross-system workflows (BPM and CCM), and implement an AI/IoT operational layer (MLOps and device telemetry) to reduce clinician burnout, improve throughput, and protect financial margin.
1. Provider Workflows — A Taxonomy
2. EHR Connectors: The Glue Across Multi-Vendor Estates
3. EHR Archival Management (Legacy Clinical Data Lifecycle)
4. Diagnostics & LIMS: Bridging Labs, Outpatient Centers and the EHR
5. Medical Devices, PACS, DICOM and Imaging Data Flows into the EHR
6. IoT, RTLS and Device Telemetry: Operational Use-Cases
7. AI, GenAI and MLOps: Clinical & Operational Use-Cases
8. Integration Patterns, Standards & Middleware (FHIR, HL7, DICOM)
9. Technology Stack and Vendor Landscape
10. GHIT Digital POV: Implementation Playbook & Accelerators
11. KPIs, Governance, Compliance and Risk
12. Deliverables, Diagrams and Closing Remarks
Provider workflows are broad and interdependent. The following taxonomy frames the integration and automation efforts GHIT Digital pursues with clients.
- Pre-admission / Scheduling / Registration: appointment booking, pre-certification, eligibility checks
- Admission / ADT: bed management, triage, encounter creation in the EHR
- Clinical Documentation & CPOE: physician orders, nursing documentation, medication administration
- Diagnostic Workflows: Laboratory (LIS), Imaging (order → modality → PACS → report → EHR)
- Point-of-Care / Bedside: telemetry, bedside vitals, infusion pumps
- Procedural / OR Workflows: scheduling, instrument and implant tracking, anesthesia records
- Recovery / Discharge / Care Transitions: discharge summaries, ePrescribe, referrals
Rapid triage, urgent diagnostics, imaging prioritization, and boarding management.
- Revenue Cycle Management (RCM): eligibility, coding, claims, denials, AR
- Supply Chain & Inventory: consumables, implants, pharmacy stock
- Asset Management & RTLS: equipment tracking and lifecycle
- Workforce Management: staffing, credentials, time & attendance
- Population Health / Care Management: registries, gap closure, chronic care
Large health systems often inherit multiple EHR platforms during acquisitions. A flagship hospital may run Epic while an acquired facility uses Cerner, and outpatient clinics may use eClinicalWorks, Athenahealth, or Meditech. CIOs and CMIOs require a unified patient view and consistent clinical workflows without disrupting billing, compliance, or legal continuity.
- Identity resolution across systems
- Encounter reconciliation between ADT platforms
- Master event routing to determine authoritative systems
- Real-time and batch synchronization of medications, allergies, problems, labs, and imaging references
- API façades exposing canonical FHIR access for applications and analytics
- Federation: Each EHR remains authoritative locally; the connector provides a unified federated view.
- Phased Migration: Selective synchronization (e.g., medications, problem lists) during planned consolidation.
- Hybrid Coexistence: Long-term coexistence with unified indexing and search.
Large integrators such as Accenture, Cognizant, and Deloitte, as well as specialist partners like GHIT Digital, provide connector frameworks with pre-built mappings, identity resolution engines, and FHIR façades for platforms such as Epic, Cerner, and Meditech.
- Reduced clinician cognitive load with unified longitudinal views
- Minimized disruption during mergers and acquisitions
- Controlled migration while maintaining billing and compliance continuity
Decades of clinical data must remain accessible for care and compliance even as legacy systems are retired. Retaining historical data in active EHRs increases cost and complexity.
- Ingest and index historical encounters, documents, images, and structured data
- Provide fast, patient-centric retrieval via embedded viewers or FHIR APIs
- Enforce retention policies, consent controls, audit trails, and legal holds
- Enterprise Content Management (ECM) systems such as OpenText, NewgenOne, and vendor archival modules
- Warm vs. cold archival tiers based on access frequency
- Embedded viewers or FHIR/REST integration
- Define retention schedules by record type
- Govern discoverability in active workflows
- Monitor performance, storage tiers, and deduplication
- Laboratory Information Systems (LIS/LIMS) manage orders, specimen workflows, results, and quality control
- Connectivity via HL7 v2 ORU messages, FHIR DiagnosticReport or Observation resources, or file transfer
- Identity and order reconciliation ensure correct encounter mapping
- Secure gateways, queues, and reconciliation workflows maintain reliability
Benefits: Faster turnaround, better auditability, and analytics for utilization and abnormal patterns.
- Imaging modalities output DICOM files routed to PACS/VNA
- Radiology reports delivered to EHR via HL7 or FHIR
- AI services integrate with PACS for inference and alerting
- Telemetry supports operational dashboards and predictive maintenance
- Asset tracking (beds, pumps, wheelchairs)
- Condition monitoring and predictive maintenance
- Patient flow tracking
- Staff safety and workflow coordination
RTLS technologies include RFID, BLE, and UWB, integrated via event-driven messaging and BPM workflows.
- Imaging AI, predictive analytics, and risk stratification
- GenAI summarization for documentation and prior authorization
- RCM automation for denial prediction and appeals
- MLOps for model governance, drift detection, and clinician feedback
- Standards: HL7 v2, DICOM, FHIR, IHE
- Middleware: Mirth Connect, Rhapsody, InterSystems, API gateways, Kafka/event hubs
- EHR Connector Layers: identity resolution and encounter reconciliation
- Clinical Backbone: Epic, Oracle Cerner, Meditech, eClinicalWorks
- Imaging: PACS + VNA (GE, Philips, Siemens) + AI
- Integration: InterSystems, Mirth, API gateways
- EHR Connector: frameworks from Accenture, Cognizant, Deloitte, GHIT Digital
- Archival Management: NewgenOne, OpenText
- Device Layer: MDI gateways, RTLS providers
- Low-Code Platforms: NewgenOne, Pega, Appian
- Analytics & ML: Snowflake, Databricks, Azure Synapse
- RCM Platforms: Optum, Trizetto, R1, FinThrive
GHIT Digital provides pre-built mappings, connectors, and accelerator kits across domains.
- Data-first integration fabric (FHIR façade + canonical data lake)
- Low-code orchestration for clinician-driven workflows
- AI operationalization (MLOps + telemetry)
- Phase 0 (0–30 days): Discovery and value mapping
- Phase 1 (30–90 days): Integration backbone and quick wins
- Phase 2 (3–6 months): AI and RTLS pilots
- Phase 3 (6–12 months): Scale orchestration, archival strategy, and governance
- EHR connector templates
- FHIR façade and identity engine
- PACS ↔ AI adapters
- LIMS workflows
- Archival ingestion and viewer kits
- Clinical: time-to-diagnosis, report turnaround, sepsis response
- Operational: MRI utilization, asset search time, OR on-time starts
- Financial: days in AR, denial rate, net collection rate
- Adoption & Safety: clinician time per patient, alert fatigue, AI accuracy
- HIPAA and device security
- AI validation and explainability
- Retention and legal hold compliance
- Executive white paper
- Integration and architecture blueprint
- Workflow swimlanes (top 10 processes)
- 90-day pilot plan with KPI dashboard
- Change management and adoption playbook
- Integration fabric
- Imaging and AI chain
- Archival data flow
Closing Remark: Provider success depends on practical interoperability, archival discipline, and operational AI that is explainable and embedded into clinical workflows. GHIT Digital combines domain expertise with accelerators and change management to drive outcomes for P2 organizations.
#GHITDigital #ProviderTransformation #HealthcareIT #EHRConnectors #EHRArchive #FHIR #PACS #ImagingAI #IoT #RTLS #RCM #NewgenOne #LowCode #GenAI
Contact:
GHIT Digital — Digital Transformation & Healthcare Integrations
Email: contact@ghitdigital.com