Severity: Warning
Message: fopen(/home/pw4h7jd5oxft/public_html/ghit.digital/application//temp/ci_session_frontende2b109dd8de872cc1a2f529344bf54e6601937cc): failed to open stream: Disk quota exceeded
Filename: drivers/Session_files_driver.php
Line Number: 172
Backtrace:
File: /home/pw4h7jd5oxft/public_html/ghit.digital/application/third_party/MX/Loader.php
Line: 173
Function: _ci_load_library
File: /home/pw4h7jd5oxft/public_html/ghit.digital/application/third_party/ion_auth/libraries/Ion_auth.php
Line: 64
Function: library
File: /home/pw4h7jd5oxft/public_html/ghit.digital/application/third_party/MX/Loader.php
Line: 173
Function: _ci_load_library
File: /home/pw4h7jd5oxft/public_html/ghit.digital/application/third_party/MX/Loader.php
Line: 192
Function: library
File: /home/pw4h7jd5oxft/public_html/ghit.digital/application/third_party/MX/Loader.php
Line: 153
Function: libraries
File: /home/pw4h7jd5oxft/public_html/ghit.digital/application/third_party/MX/Loader.php
Line: 65
Function: initialize
File: /home/pw4h7jd5oxft/public_html/ghit.digital/application/third_party/MX/Base.php
Line: 55
Function: __construct
File: /home/pw4h7jd5oxft/public_html/ghit.digital/application/third_party/MX/Base.php
Line: 60
Function: __construct
File: /home/pw4h7jd5oxft/public_html/ghit.digital/application/third_party/MX/Controller.php
Line: 4
Function: require
File: /home/pw4h7jd5oxft/public_html/ghit.digital/application/third_party/MX/Modules.php
Line: 123
Function: include_once
File: /home/pw4h7jd5oxft/public_html/ghit.digital/application/core/MY_Controller.php
Line: 9
Function: spl_autoload_call
File: /home/pw4h7jd5oxft/public_html/ghit.digital/index.php
Line: 315
Function: require_once
Severity: Warning
Message: session_start(): Failed to read session data: user (path: /home/pw4h7jd5oxft/public_html/ghit.digital/application//temp)
Filename: Session/Session.php
Line Number: 143
Backtrace:
File: /home/pw4h7jd5oxft/public_html/ghit.digital/application/third_party/MX/Loader.php
Line: 173
Function: _ci_load_library
File: /home/pw4h7jd5oxft/public_html/ghit.digital/application/third_party/ion_auth/libraries/Ion_auth.php
Line: 64
Function: library
File: /home/pw4h7jd5oxft/public_html/ghit.digital/application/third_party/MX/Loader.php
Line: 173
Function: _ci_load_library
File: /home/pw4h7jd5oxft/public_html/ghit.digital/application/third_party/MX/Loader.php
Line: 192
Function: library
File: /home/pw4h7jd5oxft/public_html/ghit.digital/application/third_party/MX/Loader.php
Line: 153
Function: libraries
File: /home/pw4h7jd5oxft/public_html/ghit.digital/application/third_party/MX/Loader.php
Line: 65
Function: initialize
File: /home/pw4h7jd5oxft/public_html/ghit.digital/application/third_party/MX/Base.php
Line: 55
Function: __construct
File: /home/pw4h7jd5oxft/public_html/ghit.digital/application/third_party/MX/Base.php
Line: 60
Function: __construct
File: /home/pw4h7jd5oxft/public_html/ghit.digital/application/third_party/MX/Controller.php
Line: 4
Function: require
File: /home/pw4h7jd5oxft/public_html/ghit.digital/application/third_party/MX/Modules.php
Line: 123
Function: include_once
File: /home/pw4h7jd5oxft/public_html/ghit.digital/application/core/MY_Controller.php
Line: 9
Function: spl_autoload_call
File: /home/pw4h7jd5oxft/public_html/ghit.digital/index.php
Line: 315
Function: require_once
By GHIT Digital
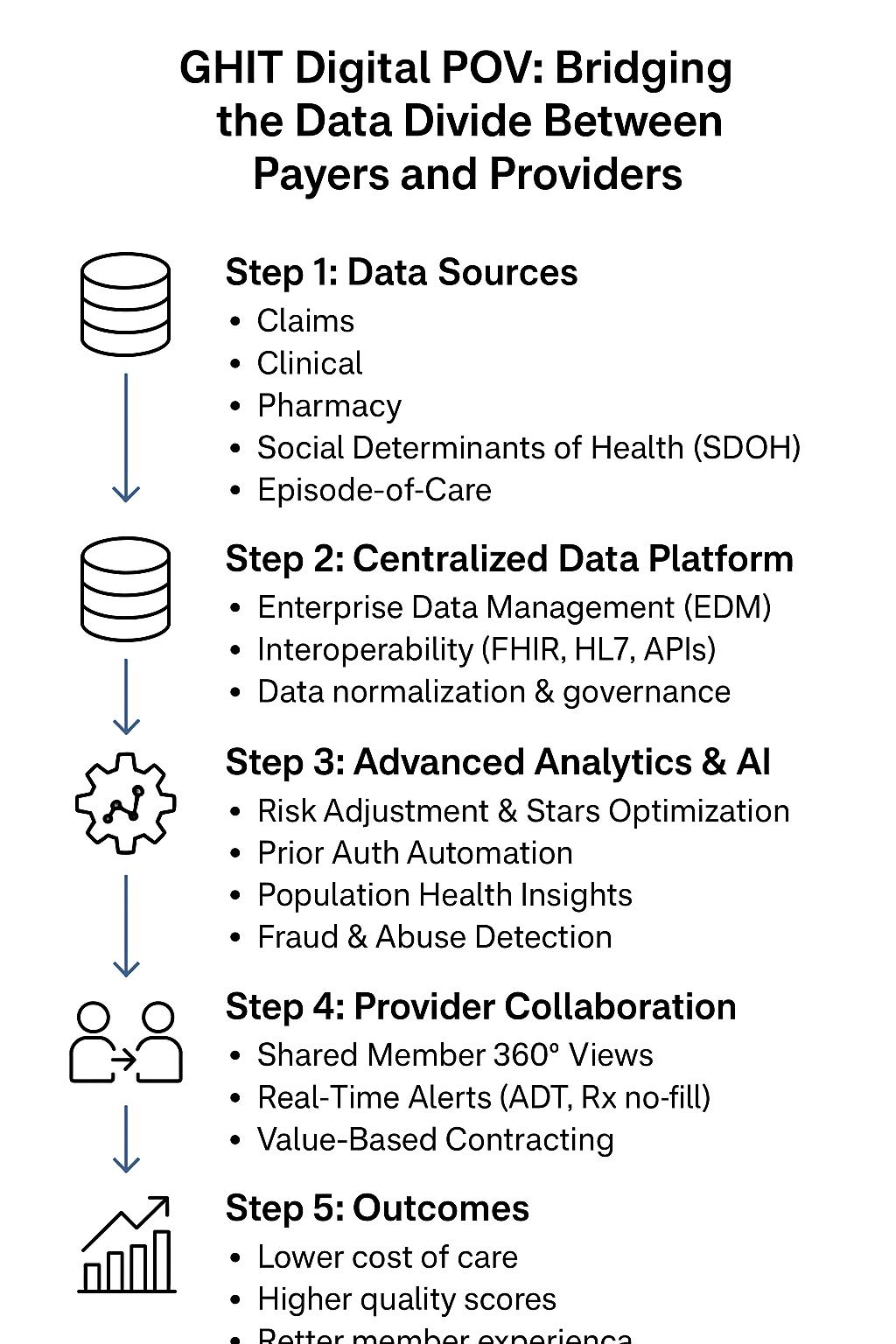
The U.S. healthcare ecosystem is at a crossroads. Payers and providers are under immense pressure from regulatory reform, rising costs, and the accelerating shift toward value-based care (VBC). Yet one persistent challenge continues to undermine transformation: the inability to integrate claims, clinical, pharmacy, and social determinants of health (SDOH) data into a unified, actionable foundation.
While many payers have invested in data sharing capabilities, true integration remains elusive. This gap prevents the industry from realizing the full potential of AI, automation, and predictive analytics to drive population health outcomes, operational efficiency, and member satisfaction.

Recent research reveals the paradox:
This is more than a technical gap; it is a structural misalignment between payers and providers.
Without integration, the insights remain fragmented—limiting both operational efficiency and patient outcomes.

For providers, the Electronic Health Record (EHR) is the system of truth. For payers, the equivalent must be a Member 360 profile that integrates:
This holistic, longitudinal record enables risk stratification, predictive modeling, and personalized member engagement at scale.

AI adoption across payers is still below 20%, largely due to incomplete data foundations. But once integration is achieved, AI-first operations become possible.

Historically, payers and providers have had adversarial relationships—contract negotiations, reimbursement disputes, and data silos. But under delegated risk, capitation, and VBC contracts, collaboration is no longer optional.
When both sides align, the result is a win–win: lower costs, improved outcomes, and sustainable margins.

??
??
??
??

At GHIT Digital, we believe that data integration is the foundation of payer transformation. Our team helps payers and providers:
The future belongs to payers who can transform fragmented data into integrated insights, and then into member-centric, outcome-driven actions.

The payer–provider relationship is shifting from transactional to transformational. By investing in centralized data platforms, AI-driven workflows, and real-time collaboration, healthcare organizations can bridge the divide between financial management and clinical excellence.
In doing so, they unlock the promise of value-based care, population health management, and sustainable healthcare economics.

Hashtags | Key Words
#Healthcare #Payers #Providers #ValueBasedCare #AIinHealthcare #HealthcareData #Interoperability #PopulationHealth #CareManagement #PharmacyAnalytics #RiskAdjustment #PriorAuthorization #FraudDetection #HealthcareInnovation #GHITDigital
We should connect. We could talk about market trends and explore business synergies, if any.
Monika Vashishtha, MBA, ITIL, PMP
President & COO
https://ghit.digital I +1 201.792.8924