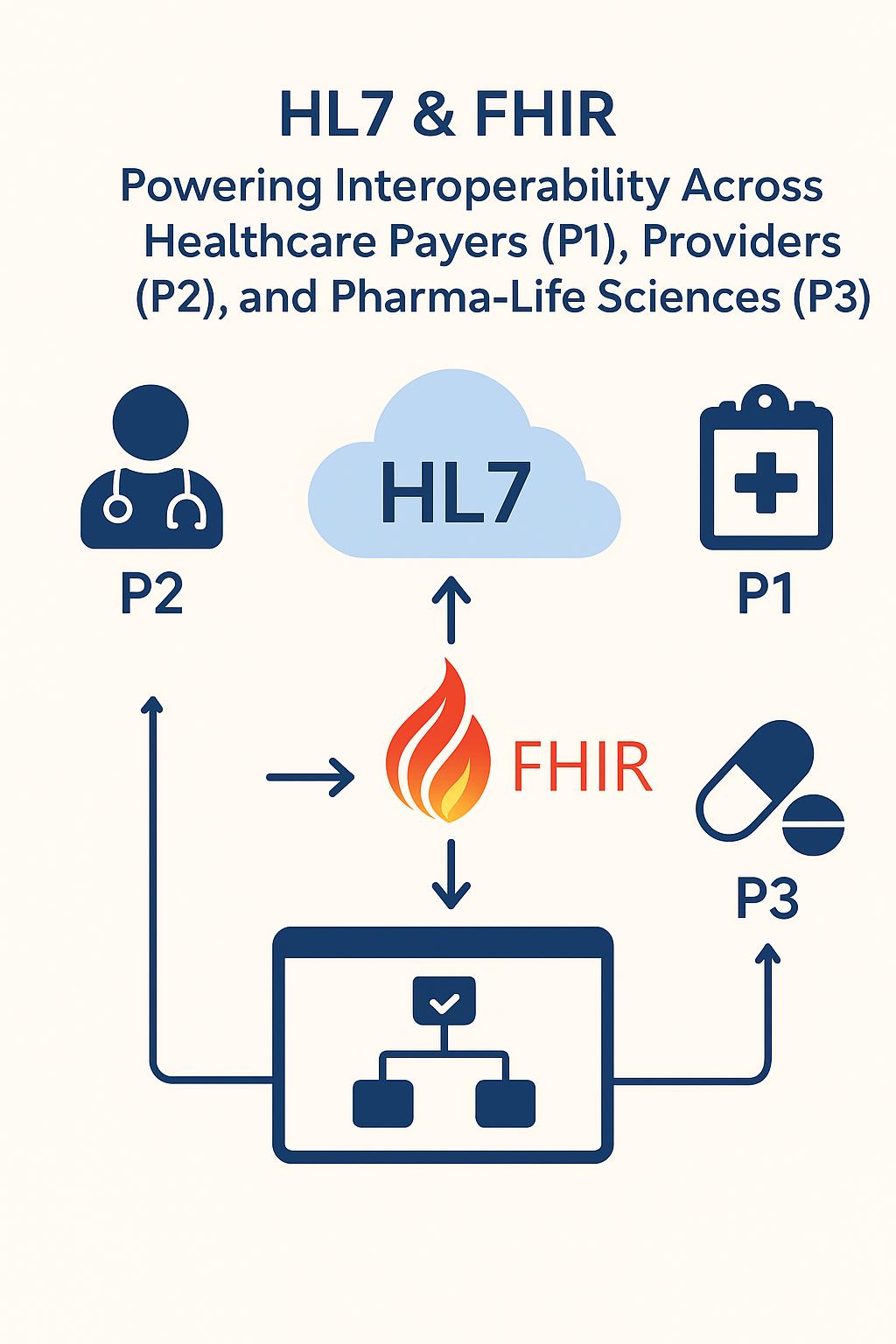
From HL7 to FHIR: The Interoperability Journey and Why It Matters Now
From HL7 to FHIR: The Interoperability Journey and Why It Matters Now
For Payers (P1), Providers (P2), Pharma / Life Sciences / Medical Devices (P3)
-
1. Executive Summary
Healthcare interoperability has evolved from HL7 v2 pipelines to FHIR-based APIs. Modern healthcare demands real-time, app-driven, API-first data exchange. Strategic interoperability is essential for care continuity, regulatory compliance, analytics, and real-world evidence generation.
-
2. HL7: The Foundation of Clinical Interoperability
-
2.1 HL7 v2 Growth
- - Lightweight, text-based protocol (pipe-delimited).
- - Event-driven: ADT, ORU, ORM, DFT, MDM.
- - Asynchronous messaging with ACK/NACK.
- - Ubiquitous in EHRs, labs, radiology, devices.
-
2.2 Limitations
- - Hard to orchestrate and scale for multi-consumer ecosystems.
- - No query model; dependent on event pushes.
- - Semantic inconsistencies (custom Z-segments).
- - Poor web/REST integration; JSON/modern formats absent.
HL7 was a hero of its time, but 21st-century digital healthcare exposed its limits.
-
3. FHIR: The API-First Future
- - Resource-oriented model (Patient, Observation, Encounter, Claim).
- - RESTful APIs with JSON/XML support.
- - Profiles & constraints (US Core, CARIN) ensure standardization.
- - Security via SMART on FHIR, OAuth2, OpenID Connect.
- - Provenance, versioning, extensions for traceability.
Timeline: DSTU 1 → R4 → regulatory push → cloud adoption (AWS, Azure, Google Health API).
-
4. Why Interoperability Matters Now
Drivers for P1/P2/P3 with examples:
| Stakeholder |
Drivers & Use Cases |
| P2 – Providers |
Longitudinal care, SMART apps, avoid duplicate testing, rapid onboarding |
| P1 – Payers |
Consumer access, value-based analytics, provider engagement, integrated claims/clinical workflows |
| P3 – Pharma / Med Devices |
Real-world evidence, trial site integration, device telemetry, post-market surveillance |
-
5. HL7 + FHIR: Bridging Generations
Hybrid architecture pattern:
- 1. Legacy HL7 pipelines remain for mission-critical flows.
- 2. Canonical FHIR repository (FPDR) layers on top.
- 3. Integration engine ingests HL7 → FHIR.
- 4. Expose SMART on FHIR endpoints for apps, analytics, partner systems.
- 5. Gradual migration of new integrations directly to FHIR.
- 6. Governance ensures stability and compliance.
-
6. Use Cases
- 1. Cross-organization patient summary (P2 + P3)
- - HL7: CCD/CCDA transfers
- - FHIR: GET /Patient/{id}/$everything → normalized data
- - Benefit: continuity, fewer errors, smoother transitions
- 2. Consumer access to claims + clinical (P1)
- - HL7: custom glue required
- - FHIR: FPDR + SMART app → unified, real-time view
- - Benefit: regulatory compliance, better UX
- 3. Real-world evidence / clinical trial data (P3)
- - HL7: scattered, inconsistent data
- - FHIR: bulk queries / subscription → normalized RWE
- - Benefit: consistent longitudinal data for analysis
- 4. Provider-payer coordination (P1 + P2)
- - HL7: faxes, batch files
- - FHIR: Task / communication resources → proactive, closed-loop care
- - Benefit: tighter care coordination, reduced friction
-
7. Architecture & Technical Patterns
- - Hybrid HL7 + FHIR
- - Event-driven subscriptions, bulk data export, SMART app integration
- - Security: OAuth2 scopes, access auditing
- - Governance: version control, semantic validation
-
8. Strategic Implications & Recommendations
Faster onboarding, AI/analytics readiness, compliance, improved patient/provider experience
- Recommended steps:
- 1. Adopt hybrid HL7 + FHIR architecture
- 2. Implement canonical FHIR repository
- 3. Build SMART-on-FHIR enabled apps
- 4. Leverage cloud FHIR platforms
- 5. Enforce governance and continuous monitoring
-
9. Conclusion
HL7 and FHIR complement each other. Organizations that adopt this hybrid approach gain operational, regulatory, and clinical advantages across payers, providers, and life sciences.